What Does Health Care For All Look Like?
October 14, 2021 10:45 pm Leave your thoughtsBy Becca Mohally Renk
[Becca Mohally Renk has lived in Ciudad Sandino, Nicaragua, for 20 years, working with the Jubilee House Community and its project, the Center for Development in Central America. The JHC-CDCA has been in Nicaragua since 1994 working in sustainable community development and runs a full time health clinic in Nueva Vida. Becca and her husband Paul have two daughters in 9th and 10th grades in public school in Nicaragua.]

I’d like you to imagine for a moment that you are the parent of a child with asthma, living in Ciudad Sandino, just outside the capital of Nicaragua, in a barrio called Nueva Vida, which was recently founded after your family – along with 1,200 other families – was flooded out of your home along the lakeshore in Managua during Hurricane Mitch. The year is 2001, and although your family now has a concrete house and the bus runs regularly down your street in the daytime, nights are filled with rival gangs throwing rocks and bottles, and regular work has been nearly impossible to find. These days, you travel into the market in Managua before dawn to wash potatoes for a vegetable seller; with what you earn, you can usually bring home a little food for your family’s lunch. Although you have five children, it’s your middle child, the seven year-old, who worries you the most. She suffers from asthma, and you haven’t been able to save up to buy the expensive inhalers she needs to stop her persistent wheezing. Tonight, while your family is trying to sleep, smoke from burning trash in the nearby dump is heavy in your home, and your daughter can’t breathe. In the half-light you can see her eyes wide, struggling with an asthma attack. All you can think is that you have to help her. You don’t have a motorcycle, let alone a car, and the buses don’t run at this hour. You load your daughter onto the crossbar of your bicycle and ride through darkened streets – going around the long way to avoid the gangs – until you arrive at the Hospitalito. Although it’s called the little hospital, it’s really just a clinic. The doctor on duty is distressed when you arrive, he listens to your daughter’s lungs and sadly tells you that he has no medicine, no inhaler, no nebulizer, no tools to help you. Your daughter must go to a larger hospital in Managua, but there is no ambulance to take her. So you set her, weak and wheezing, on the curb, and begin to beg passersby for bus fare as light dawns over the useless hospital.
Life under the neoliberal governments in Nicaragua – 1990-2006 – was exceptionally hard. In those years, the poor got poorer and the rich got richer and Nicaragua became one of the most unequal countries in the world. Lack of access to basic health care was one of the ways in which everyday people suffered.
Under the Somoza dictatorship in 1978, there were a total of 209 health units in the country – that is hospitals, health centers and health posts combined. After the Triumph of the Revolution in 1979, the new Sandinista government made health care free, and even in the midst of an economic embargo and fighting the Contra War during the 1980s, they managed to increase health units five-fold; by 1990 there were 1,056 units. But during 16 years, the neoliberal governments only managed to build 35 more health units, the majority of which were in rural areas and sat empty due to lack of personnel and materials.
One of these units was our “Hospitalito,” in Ciudad Sandino. At that time, the public budget for medicines and materials was minimal: when the doctors who were working at our clinic during the day took the night shift at the Hospitalito, they had to turn sick people away because they didn’t even have gloves to examine patients or basic medicines. Even when patients managed to be seen by a doctor, they were given prescriptions for medicines they couldn’t afford. Imports of drugs were in the hands of foreign companies and production of generic drugs was restricted. Patients unfortunate enough to need surgery had to bring their own alcohol, gauze, sutures and sheets – oh, and also family members who could donate the blood they would need. Laboratory tests, specialized treatments, and surgeries were so expensive that poor families effectively could not access the service. During these years, patients literally died on the street outside hospitals for lack of basic medical care.
Since the return of the Sandinista government in 2007, the difference in medical care is stark. Today, the Hospitalito is a fully equipped hospital with emergency care and admitted patient beds. There is outpatient care – general medicine, pediatrics, gynecology, psychology, natural medicine, a rehabilitation center, and a maternal wait home.
Ciudad Sandino is just one city – public health care has been revolutionized all over the country, the entire structure and indeed culture of the health system has changed. Today, it is a more holistic system focused on families becoming active participants in their own health, and relying heavily a small army of community workers doing everything from mosquito elimination to door-to-door vaccination to health promotion and education.
Since 2007, the largest public health infrastructure in Central America has been built, now with a total of 1,565 health units. In 14 years, Nicaragua has built 21 new hospitals and remodeled 46 more. It has built or remodeled 1,259 medical posts, 192 health centers and 178 maternity homes. In an effort to see patients who don’t normally go to health centers, MINSA also has 66 fully-equipped mobile health clinics. These are made from semi trucks that have been confiscated in drug busts, and converted into clinics; in 2020 these mobile clinics provided nearly 1.9 million consults. In the midst of the pandemic, MINSA rolled out the My Hospital in My Community program which sees patients at neighborhood health fairs with orthopedists, cardiologists, gynecologists and urologists and includes screening for prostate, breast and cervical cancers. Patients are then referred to a specialist at a hospital for follow up.
Access to specialized care has drastically changed – services such as chemotherapy and radiotherapy that were once only offered in the capital are now offered at regional hospitals. Prior to 2007, many surgeries were only performed by international brigades; last year 120 child heart surgeries and 4 kidney transplants were performed, all by local doctors. This year, Nicaraguan doctors became the first team in Central America to perform in-utero surgery, on a fetus with spina bifida.
The list of improved health services is comprehensive by any standards: 260,000 cataract surgeries, care of 358,000 older adults and people with disabilities, three prosthetics and orthotics workshops, 91 centers for people with special needs, 265 free daycare centers, and 188 natural medicine clinics, 72 pain clinics, 34 mental health clinics integrated into existing public health centers.
Nicaragua has made a long term financial investment in public health: in 2020, 40 cents of every dollar the government spent was for health care and education. Nicaragua now spends 476% more on health than previous governments, investing 5.2% of its GDP in the sector annually.
In 14 years, total number of health care workers employed in the public sector is up by 66%, doctors up by 123%, free medical consultations are up by 329%, All this, combined with the school lunch program which guarantees a hot meal of beans and rice to 1 ½ million primary school children daily, has resulted in a 46% reduction in chronic malnutrition in children under five and a 66% reduction in chronic malnutrition in children six to 12 years old.
Investment leads to results: a 385% increase in pap tests plus equipping clinics with colposcopy and cryotherapy machines has led to a 25% decrease in cervical cancer mortality, previously one of the biggest killers of Nicaraguan women of child-bearing age.
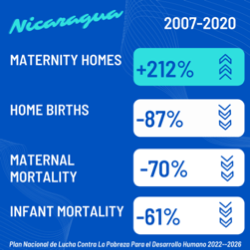
A 212% increase in maternal wait homes has led to an 87% decrease in home births, followed by a 70% decrease in maternal mortality over the more than 1.5 million births attended since 2007, and a 61% reduction in infant mortality.
Moving forward, Nicaragua plans to continue expansion – finishing five more new hospitals before the end of the year, building 12 more new by 2026 and continuing hospital remodeling as well.
It is in this context of more than a decade of these revolutionary changes to the health care system that Nicaragua faced the coronavirus. When COVID-19 was declared a pandemic, Nicaragua was already prepared by having a healthier population with access to the best public healthcare in the region.
To date, it has seen fewer cases and fewer deaths than any country in the region; in fact, it compares favorably to the most developed countries in the world. Nicaragua has achieved this by refusing to carbon copy the approach of the developed world like the rest of the region as done – with lockdowns, strictly enforced curfews, and school closures – but rather choosing to fight the pandemic on its own terms, with a strategy devised for Nicaraguan reality. The government recognized that in a country where most people depend on daily earnings to survive, lockdown would result in hunger; that with children depending on their free school lunch for vital nutrition, school closures would result in hunger; and that with the economy already suffering from the failed coup attempt in 2018 (damages are estimated to be equivalent to that of 52 hurricanes like Eta and Iota which hit Nicaragua in 2020), forced economic shut down would cripple the nation. Instead, the government strategy to fight the pandemic played to Nicaragua’s strengths: its well-organized community health system and resilient population.
From late March 2020 when the first coronavirus case in the country was confirmed, through mid-May when the first wave began to peak, lay health promoters carried out 5 million home visits to the country’s 1.3 million homes to share information on the virus, go through symptom checklists and identify possible cases. The public was encouraged early on to learn to live with the virus by going about their business safely, something the international scientific community is now also promoting as the world begins to recognize it is moving from pandemic to endemic COVID-19.
Nicaragua’s adaptation has been agile and widespread: schools, markets, shops, taxis and bus cooperatives came up with creative hand-washing ideas right away. [Editor’s note: This was when doctors still thought the virus could be passed through touching surfaces.] The population adapted to wearing masks in crowded areas early on, and we did not see a politicized mask debate. Unlike in countries where the government has made decisions for people what is safe and what is not, Nicaraguans have learned to judge for themselves what is safe, and life has continued.
Nicaragua’s softer approach has resulted in fewer COVID cases than any country in the region, and its economy is in better shape. Nicaragua was forecast to have a 14% loss of its GDP in 2020, but managed only a 2% loss and was the only country in Central America to increase its exports in 2020. Even when adjusting for “excess” deaths – those above the expected death rate – Nicaragua has not only fared better in the pandemic than any other country in the region, but also larger countries like the U.S. and U.K.
Unlike the developing world, the Nicaraguan response has never relied on testing – due to cost and lack of reagents, testing has been necessarily limited; but we also know that testing is also slow and unreliable. Although COVID tests are available – mostly for those who require it for traveling outside the country, at a cost of $150 per test – the current public health protocol calls for only testing at-risk patients: pregnant women, the elderly and healthcare workers. Rather than waiting for a test-confirmed diagnosis, any patient presenting even one symptom is treated as a suspected case. Recently, a member of our community got COVID, so we saw up close what happens when a patient is sick. When she first got a fever and aches, she called the free hotline to ask what to do. The doctors told her to go to the Hospitalito. She was examined and, like all patients with suspected COVID, was given two specific medications, plus others as needed in accordance with her own medical history. She was told to isolate at home for 14 days and come back if she presented more symptoms. Patients are also asked who they have been in contact with, and those contacts are then visited by health care workers, given a round of prophylactic medicines and told to come to see a doctor if they present more symptoms.
In the area of prevention, Nicaragua is vaccinating against COVID-19, but the rollout has been slower than hoped for due to a lack of vaccines. This is especially frustrating because Nicaragua knows how to vaccinate: this country created the internationally used model for how to vaccinate in war zones when it eradicated polio and other childhood diseases with its vaccination campaign during the Contra war in the 1980s. Since 2007, Nicaragua has maintained a nearly universal vaccination rate, and public health workers participate in annual vaccination campaigns door to door throughout the country. Even in the first months of the pandemic, 2 million people were vaccinated against influenza and pneumonia with vaccines made at a lab in Nicaragua.
But, as we have seen around the world, the COVID vaccine rollout is not equal and has been politicized with what is being called “vaccine diplomacy.” The United States – where to date 15 million unused vaccines have been thrown out, enough to vaccinate every Nicaraguan twice – has donated vaccines to every other Central American county except Nicaragua.
Since March, Nicaragua has been vaccinating for free, starting with oldest population – those over 30 are currently eligible. So far, more than half a million people have been vaccinated, with the goal of doubling that by October 9th. Although there was initially some vaccine hesitancy in the older population, as COVID cases have risen in recent weeks, demand for the vaccine has also risen. Fortunately, the health care system’s organization is up to the task of dealing with long lines: I recently went to one of the five hospitals in Managua offering the vaccine. Although I was daunted by the snaking line outside the hospital, once I joined, it moved quickly. Despite the wait, there was a jubilant mood among us all and within two hours we were jabbed and done. We estimated 10,000 people got their vaccine at that hospital that day.
In Nicaragua we are currently experiencing a second wave – which is remarkable since other countries are already on their fourth wave. With this second wave, we are also fighting what Nicaraguan Vice President Rosario Murillo calls “health terrorism,” meaning disinformation about the pandemic situation, which has been widespread during both waves. Around the world, the pandemic has been politicized, and that is especially true in Nicaragua. The USAID “regime change” plan for Nicaragua, Responsive Assistance in Nicaragua, or RAIN, which was leaked in July 2020, specifically mentions exploiting the COVID-19 pandemic into a “humanitarian emergency” through what it calls Nicaragua’s “weak healthcare system.” Even before there were reported cases in Nicaragua, we saw this playing out through manipulation of international media, scare tactics via WhatsApp messages and Facebook, and even the creation of a parallel “authority,” the Citizens Observatory for COVID-19 in Nicaragua, an organization of anonymous “interdisciplinary volunteers” with a slick website. Throughout the pandemic they have reported exaggerated “parallel” numbers; and despite the fact that they admit one of their sources is “rumors,” international media have quoted Observatory counts as if they were official numbers.
I personally have been told that hospitals have “collapsed,” there are bodies stacked in corridors, and patients being turned away, only to speak with someone who had been in that hospital or go myself and find out that simply wasn’t true. Unfortunately, this health terrorism has deadly consequences. The constant disinformation scares people, and understandably so – especially older people who remember the neoliberal years when patients did die for lack of care outside of hospitals. So instead of seeking medical care, patients are self-medicating at home, and too often go to the hospital too late and wind up much sicker or even die. To combat it, this week health care workers have again been deployed to go door-to-door checking on people, giving information, and convincing those who are sick to seek medical care.
What does the future hold? Nicaragua will keep caring for its people, plugging away to reduce inequities in health and to eradicate poverty. As President Ortega said recently, “The most terrible virus that exists on the planet is the one that causes poverty, because it is in the genes of those who dominate the world economy under capitalism. It is based on the principle of survival of the fittest, no matter how many dead it leaves in its wake.… That is savage capitalism, the most terrible disease on the planet.”
SOURCES: Gobierno de Reconciliación y Unidad Nacional: Plan Nacional de la Lucha Contra La Pobreza Para el Desarrollo Humano 2022-2026 http://www.tortillaconsal.com/tortilla/node/12471
Interview with Ivan Acosta, Nicaraguan Minister for Housing and Public Credit https://popularresistance.org/nicaragua-launches-new-plan-to-fight-poverty-and-promote-human-development/
Ministry of Citizen Power for Health Nicaragua: Advances in Health From 2007 to 2020 http://www.tortillaconsal.com/tortilla/node/11331
Categorised in: Uncategorized
This post was written by LPJAdmin
